
What is hip replacement surgery?
Hip replacement, or hip arthroplasty, is a surgical procedure where the damaged portions of the hip joint are replaced with artificial components. These prosthetics mimic the natural movement of the hip, allowing patients to regain pain-free mobility.
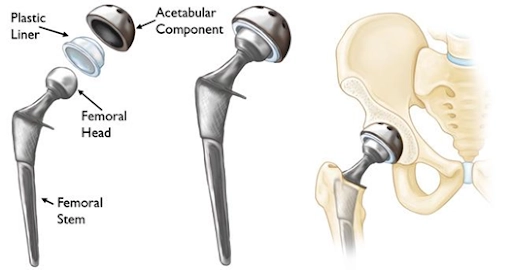
- The damaged femoral head is removed and replaced with a metal stem, which is inserted into the hollow center of the femur. The stem can be secured using either cement or a “press-fit” technique.
- A metal or ceramic ball is attached to the upper part of the stem, replacing the removed femoral head.
- The damaged cartilage lining the socket (acetabulum) is also removed and replaced with a metal socket, which may be secured using screws or cement.
- To ensure smooth movement, a spacer made of plastic, ceramic, or metal (called a liner) is placed between the new ball and socket.

What are the types of hip replacement procedures?
- Total hip replacement: Both the femoral head (ball) and acetabulum (socket) are replaced.
- Partial hip replacement: Only the femoral head is replaced, often for specific types of fractures.
- Hip resurfacing replacement: This type of hip replacement involves resurfacing the hip joint rather than fully replacing it. It is a bone-preserving procedure designed to alleviate hip pain caused by arthritis or other conditions.
- Minimally invasive hip replacement: Smaller incisions and advanced techniques for reduced recovery time and scarring.
- Revision hip replacement: Replacement of a previously implanted hip prosthesis that has worn out or failed.
How does total hip replacement surgery allow mobility and comfort?
Hip replacement surgery is a transformative procedure designed to alleviate pain, improve mobility, and enhance quality of life for individuals suffering from debilitating hip joint conditions. This advanced surgical option replaces a damaged or worn-out hip joint with a prosthetic implant, restoring function and comfort.
The hip typically moves smoothly because the ends of the bones are covered with a protective layer of tough tissue known as cartilage. When the cartilage is worn down or damaged, often due to injury, the bones begin to rub against each other, leading to pain and stiffness in the joint.
In a hip replacement, the damaged components of the hip are replaced with metal, ceramic, and plastic parts.



Who can benefit from hip replacement?
A hip replacement may be necessary if one or both of your hip joints become damaged, leading to persistent pain or difficulty with everyday activities such as walking, driving, or getting dressed.
It is most often used to relieve pain and stiffness in the hip joint caused by osteoarthritis.
Common causes of hip joint damage include:
- Osteoarthritis: Also known as “wear-and-tear arthritis,” where the protective cartilage cushioning the ends of bones within a hip joint wears away with time, causing the bones to rub against each other. This results in pain, stiffness, swelling, and reduced mobility in the affected joint. It is the most common type of arthritis and frequently affects weight-bearing joints like the knees, hips, and spine.
- Rheumatoid arthritis: An autoimmune condition where the immune system mistakenly attacks the joint lining, resulting in pain and stiffness.
- Psoriatic arthritis: A form of arthritis that is linked to psoriasis- a chronic skin condition.
- Hip fracture: Severe damage to the hip joint from a fall or similar accident may require replacement.
Other health conditions and issues that can damage your hip joint enough to require a hip replacement include:
- Avascular necrosis: a painful bone condition that can deteriorate with time caused by reduced blood supply to one of your bones. A variety of risk factors for this include a traumatic event, sickle cell disease, steroid use, alcoholism, autoimmune disorders, and hypercoagulable states.
- Femoroacetabular impingement syndrome: a condition where the hip joint’s bones are abnormally shaped causing them to rub together leading to pain and discomfort.
- Hip Dysplasia: a condition where the hip socket does not fully cover the ball portion of the upper thigh bone (femur) at the hip joint. This can cause the hip socket to be too shallow, or the ball of the hip socket to be loose or dislocated.
- Tumours: a group of abnormal cells that form lumps or growths which can start in any cells in the body and behave differently if they are cancerous (malignant) or benign (non-cancerous).
- Perthes disease: It affects the growing end of the femur bone that fits into your child’s hip socket and presents in childhood. It can cause the end of the bone to break down and then regenerate over several years.
What are the other common causes of pain in the hip region?
- Hip bursitis – Inflammation of the bursae, small fluid-filled sacs that cushion the hip joint.
- Tendonitis – Inflammation of tendons around the hip due to overuse or repetitive strain.
- Hip labral tears – Damage to the cartilage surrounding the hip socket, often from injury or repetitive motion.
- Muscle strains – Overstretching or tearing of muscles around the hip from physical activity.
- Sciatica – Pain radiating from the lower back to the hip due to compression of the sciatic nerve.
What are the benefits of hip replacement surgery?
- Pain Relief: Significant reduction or elimination of hip pain.
- Improved Mobility: Greater range of motion and ability to perform daily activities.
- Enhanced Quality of Life: Increased independence and participation in recreational activities.
- Durable Results: Modern implants often can last 15-20 years or more.
What are the alternatives to hip replacement surgery?
Most hip pain issues typically do not require surgery and can be managed with non-invasive treatments, including
- pain medication
- walking aids
- physiotherapy
- joint injections.
What happens during a hip replacement?
If you’re undergoing a hip replacement, you’ll typically be admitted to the hospital on the day of your surgery.
The procedure involves either a spinal anaesthetic, which numbs the body from the waist down while keeping you awake, or a general anaesthetic, which puts you to sleep throughout the operation.
If you opt for a spinal anaesthetic, you may also be given a sedative to help you stay calm and drowsy.
The surgery generally lasts around 1 to 2 hours, and the specific approach taken will depend on factors such as the extent of hip damage, its underlying cause, and your overall health.
The procedure involves the following steps:
- Anaesthesia: Administered to ensure comfort during surgery.
- Joint access: An incision is made to access the hip joint.
- Damaged tissue removal: The damaged cartilage and bone are removed.
- Prosthesis placement: The artificial components (metal, ceramic, or plastic) are securely placed to form a new joint.
- Closure: The incision is closed, and the area is bandaged.
What does the recovery and rehabilitation involve?
- Hospital stay: Patients typically stay in the hospital for 0-3 days.
- Pain management: Medications and physical therapy help manage postoperative pain.
- Rehabilitation: Exercises to strengthen muscles and improve joint movement start shortly after surgery.
- Return to activity: Most individuals resume normal activities within 12 weeks, with improvements continuing over several months. Improvement in pain have been shown to occur up to 1- 1.5 years following the surgery.
What are the potential risks and complications?
Your surgeon takes every precaution to minimise the risks of surgery, using state-of-the-art techniques and providing comprehensive preoperative and postoperative care.
Rest assured, your consultant will carefully assess the risks and benefits before recommending surgery.
During your initial consultation, they will also discuss any specific risks relevant to your situation.
While hip replacement is a widely successful procedure, risks are rare but possible and some of these can include:
- Infection.
- Nerve or blood vessel damage
- Blood clots.
- Implant wear or loosening over time.
- Dislocation of the prosthetic joint.
- Altered leg length
- Bone fracture
- Bone forming in muscles around the replacement
- Anaesthetic risk
What is the recovery like at home? Tips for a smooth recovery
When you return home, you may feel quite tired. Prioritise rest initially, then gradually increase your activity levels to aid recovery.
To strengthen your hip, protect it from further injury, and support wound healing, follow these guidelines:
- Perform the exercises recommended by your physiotherapist 3 to 4 times daily for 6 weeks. Listen to your body and do not worry if cannot keep up as recommended.
- Engage in low-impact activities like walking and gradually increase the distance as you feel comfortable. The balance between strengthening exercises versus walking distance should favour strengthening exercises initially, as this will allow you to achieve an increased walking distance.
- Avoid bending your hip beyond a 90-degree angle.
- Try to sleep on your back for 6-8 weeks (If unable, one can sleep on the side, using a pillow between legs, with the operative side facing upwards)
- Avoid significant twisting movements of the hip and crossing your legs.
- Refrain from lifting heavy objects or engaging in strenuous activities.
- Continue using crutches or a walking stick for support as long as needed.
- If you experience discomfort, take the prescribed painkillers until the pain subsides.
- Opt for showers instead of baths to prevent strain on your hip.
- It is critically important to keep the wound dry during healing which can take up to 3 weeks and so protect it when having a shower despite the dressing.
These steps will help ensure a safe and effective recovery.
How to maintain a healthy hip after surgery?
- Follow rehabilitation guidelines: Adhere to physical therapy and exercise routines.
- Prevent falls: Use assistive devices and take precautions to avoid accidents.
- Healthy lifestyle: Maintain a balanced diet and healthy weight to reduce stress on the joint.
- Regular check-ups: Monitor the condition of the prosthesis through routine medical evaluations.
When can I drive a car after surgery?
You may be able to drive again approximately six weeks after your surgery, although this timeframe can vary between individuals. Your surgeon will provide specific guidance on when you’re ready. Do not drive until you feel confident in controlling your vehicle and always confirm with both your surgeon and your insurance provider before resuming driving.
When can I return to work after surgery?
Before going back to work, consult your doctor for personalised advice. As a general guideline:
- Sedentary jobs (e.g. office-based work): You can typically return after 4–6 weeks.
- Mixed-labour jobs (e.g. teacher): You may return after about 3 months.
- Manual labour jobs (e.g. builder): You should wait approximately 6 months before resuming work.
How soon can you fly after hip replacement surgery?
Most surgeons and airlines recommend you should not fly within 3 months of surgery because of the increased risk of developing blood clots (Deep vein thrombosis, pulmonary embolism).
Please check with your surgeon for any advice regarding air travel and any precautions to take if you have additional risk factors for blood clots.
What is the follow-up schedule after surgery?
A wound check will be required at approximately 14 days after your surgery with a healthcare professional.
A routine follow-up appointment with your surgeon will be needed around 6–8 weeks after your surgery.
Summary: Embrace a pain-free future
Hip replacement surgery offers a reliable solution for individuals living with chronic hip pain and limited mobility. With advanced techniques and high success rates, this procedure can restore your freedom of movement and significantly enhance your quality of life. If you’re considering hip replacement, schedule a consultation to explore your options and embark on the journey to a pain-free life.
