Chondroplasty: Restoring Joint Health and Reducing Pain
Chondroplasty is a minimally invasive surgical procedure designed to repair and smooth damaged cartilage in a joint. By addressing cartilage issues early, chondroplasty can relieve pain, improve joint function, and potentially prevent further joint degeneration. This advanced procedure is most commonly performed on the knee but can also be applied to other joints like the hip or shoulder.
What is Chondroplasty?
Chondroplasty involves the surgical smoothing and reshaping of damaged cartilage surfaces within a joint. Cartilage damage can occur due to injury, overuse, or degenerative conditions like osteoarthritis. During chondroplasty, the surgeon removes frayed or loose cartilage, allowing the joint to move more smoothly and reducing irritation and pain.
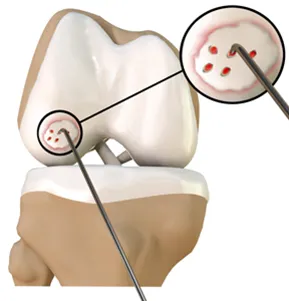
If the damage to the articular cartilage is severe and bare bone is exposed, a surgical procedure called Microfracture may be performed. This surgery is done arthroscopically and involves the surgeon creating multiple small holes in the bone at the site where cartilage is missing. These holes allow blood, rich in growth factors, to flow into the area and cover the bone surface. Over time, this blood forms a clot that gradually develops into new cartilage, known as fibrous cartilage.
Who Can Benefit from Chondroplasty?
Chondroplasty is often recommended for individuals who:
- Have cartilage damage caused by injury, wear-and-tear, or arthritis.
- Experience persistent joint pain, swelling, or stiffness.
- Have limited joint function that affects daily activities.
- Have not responded well to conservative treatments like physiotherapy or medication.
What are the benefits of chondroplasty?
- Improves pain and joint function.
- Minimally invasive with a short recovery period.
- Can delay or prevent the progression of arthritis.
- Enhances overall quality of life by restoring mobility.
How is Chondroplasty Performed?
The procedure is typically done using arthroscopy, a minimally invasive surgical technique. Here’s an overview of the process:
- Preparation: The patient receives regional or general anaesthesia.
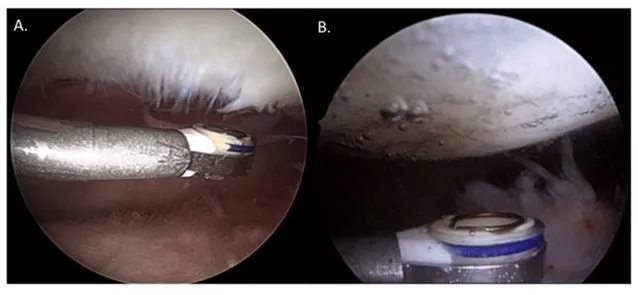
- Arthroscopic (keyhole) access: Small incisions are made, and a thin camera (arthroscope) is inserted into the joint.
- Cartilage Repair: Specialised tools are used to smooth and remove damaged cartilage.
- Microfracture: If the damage to the articular cartilage is severe and bare bone is exposed, a surgical procedure called Microfracture may be performed. This surgery is done arthroscopically and involves the surgeon creating multiple small holes in the bone at the site where cartilage is missing. These holes allow blood, rich in growth factors, to flow into the area and cover the bone surface. Over time, this blood forms a clot that gradually develops into new cartilage, known as fibrous cartilage.
- Irrigation: The joint is flushed to remove any debris, ensuring a clean and smooth surface.
The procedure usually takes 30-60 minutes and is performed on an outpatient basis.
What should I expect after surgery?
- Mobilisation: You will be encouraged to start moving on the day of your surgery, possibly with the assistance of elbow crutches, depending on the location of your repair. You should also be able to navigate stairs. The exercises you can perform will depend on the repair site and any specific restrictions set by your surgeon. Your physiotherapist will guide you through appropriate exercises before you are discharged.
- Pain Relief: A nerve block may be administered during surgery, causing temporary numbness in your limb immediately afterward. As the effect wears off, it is normal to experience some pain, for which you will be given painkillers. It is important to take them as prescribed to manage discomfort effectively. Post op pain can continue for at least 3 months given the nature of the surgery.
- Ice Therapy: Applying ice can help reduce pain and swelling. To prevent your dressings from getting wet, cover them with a plastic bag. Wrap a bag of ice or frozen peas in a damp towel and apply it to the affected area for 10–15 minutes. This can be repeated every 3–4 hours. If you have undergone knee or foot surgery, keeping your leg elevated on pillows can also aid in reducing swelling.
- Wound Care: Your wounds must be kept meticulously clean and dry till they heal which can be up to 3 weeks in most cases. The nursing staff will provide detailed wound care instructions before your discharge.
When can I return to driving?
You should not drive while using elbow crutches. Please discuss this with your consultant or physiotherapist. The timing of your return to work will depend on the nature of your job, and your physiotherapist can provide guidance based on your specific role.
When can return to sports?
Your ability to return to leisure activities and sports will depend on the extent of your surgery and the type of activities you wish to resume. Your consultant or physiotherapist will provide tailored advice on when it is safe to return to these activities.
What are the risks and potential complications?
While chondroplasty is considered safe, some of the potential risks include:
- Swelling or temporary joint stiffness.
- Infection or bleeding (rare).
- Incomplete pain relief if cartilage damage is severe.
- Blood clots (Deep vein thrombosis, pulmonary embolism)
Our skilled team uses the latest techniques to minimise risks and ensure a smooth recovery for all patients.
Summary: Why Choose Chondroplasty?
Chondroplasty is an effective solution for addressing cartilage damage early, reducing pain, and restoring joint health. This minimally invasive procedure offers:
- Quick recovery with long-lasting results.
- Improvement in pain and joint function.
- A proactive approach to managing joint health.
If you’re experiencing persistent joint pain or mobility issues, schedule a consultation today to learn if chondroplasty is the right treatment for you.
